Regulatory Pathways
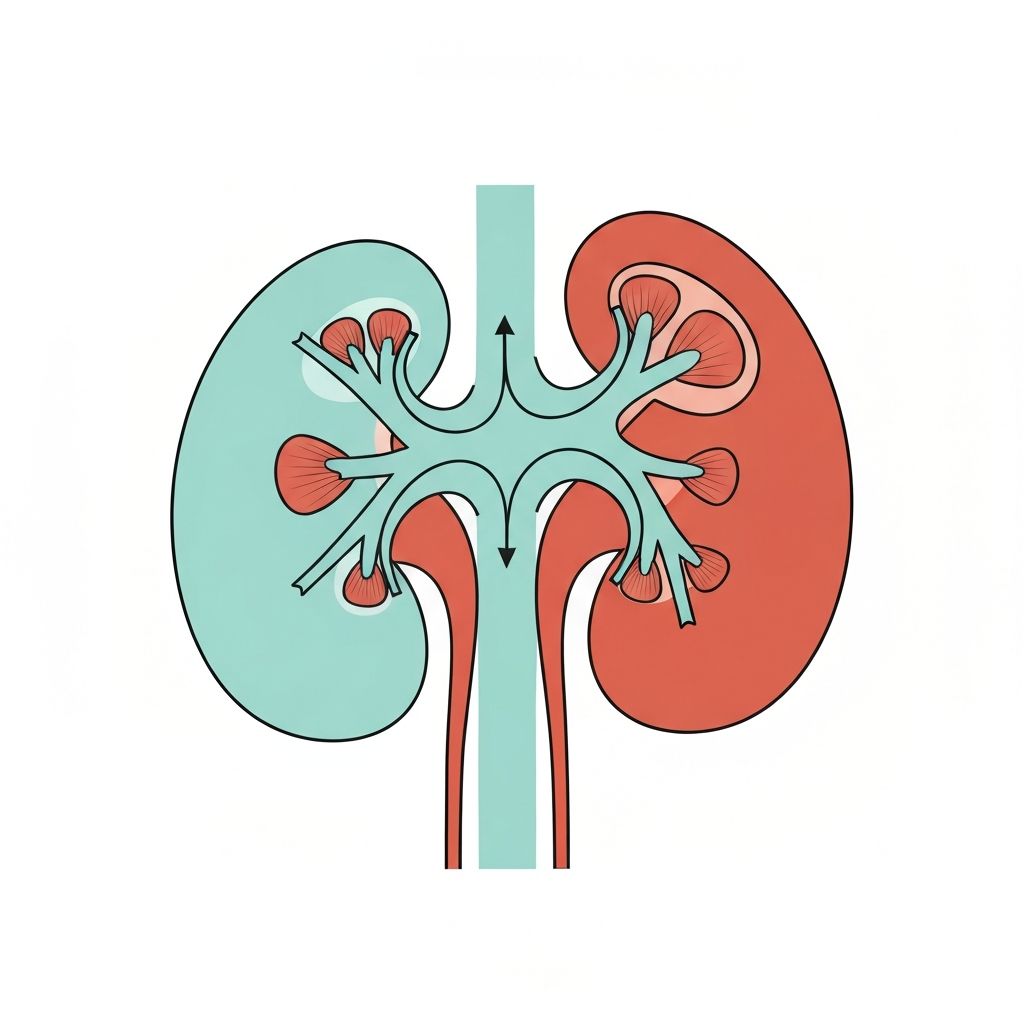
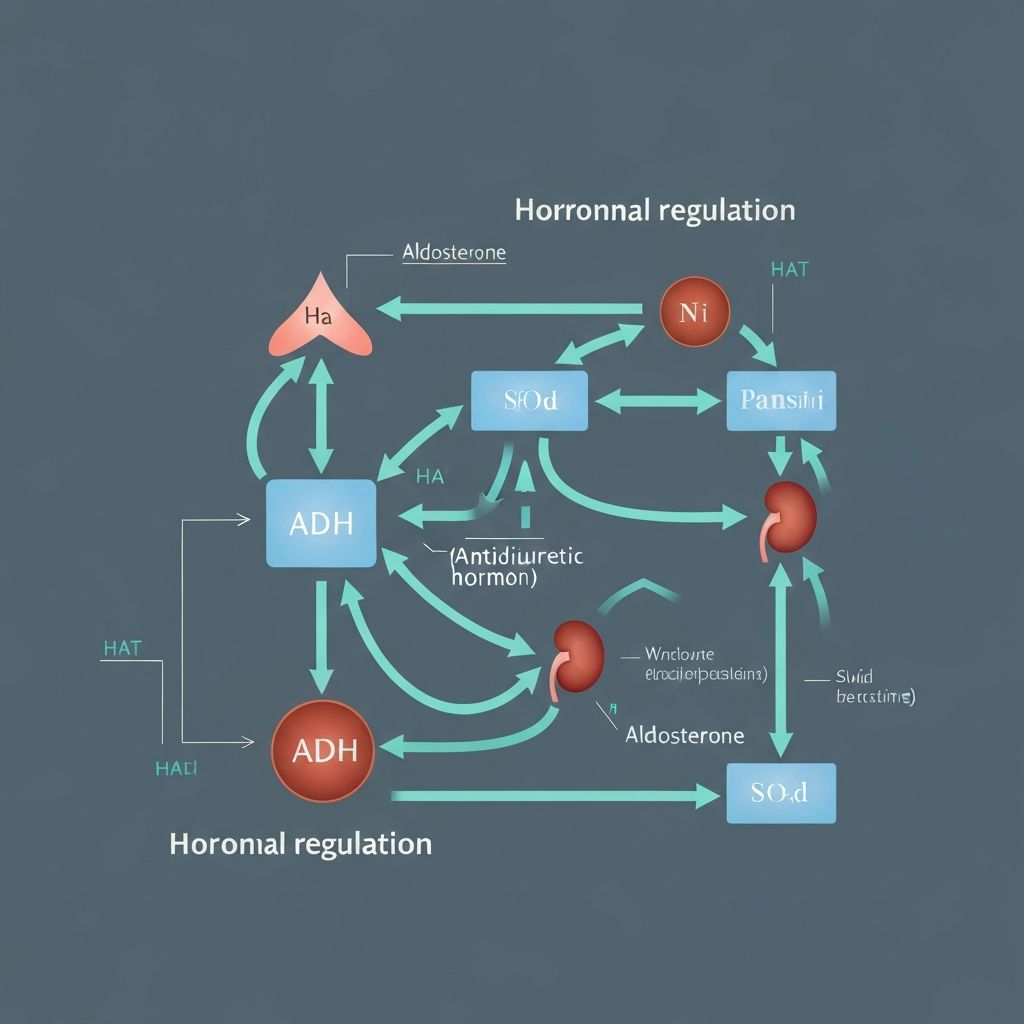
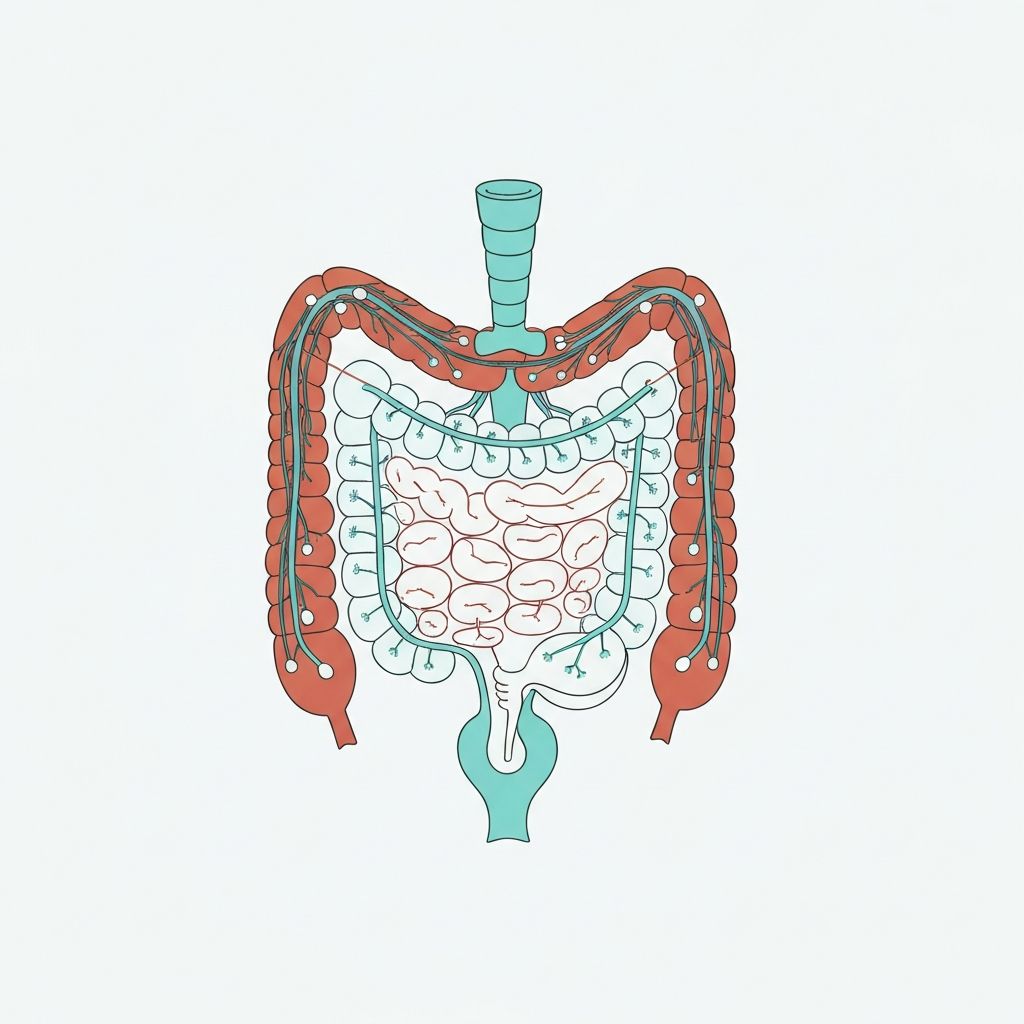
The kidneys continuously filter blood and reabsorb essential substances, including water. This process is regulated by hormones such as aldosterone and antidiuretic hormone (ADH), which respond to changes in blood osmolarity and volume. These regulatory systems ensure the body maintains appropriate fluid distribution between intracellular and extracellular compartments.